The meniscus is a crucial component of the knee joint, helping to distribute weight evenly and absorb shock during movement. Unfortunately, it is also prone to injury, particularly in athletes who engage in high-impact sports. Meniscus injuries can range from minor tears to complete ruptures, and the severity of the damage will determine the best course of action for recovery.
Understanding the Meniscus
Anatomy of the Meniscus
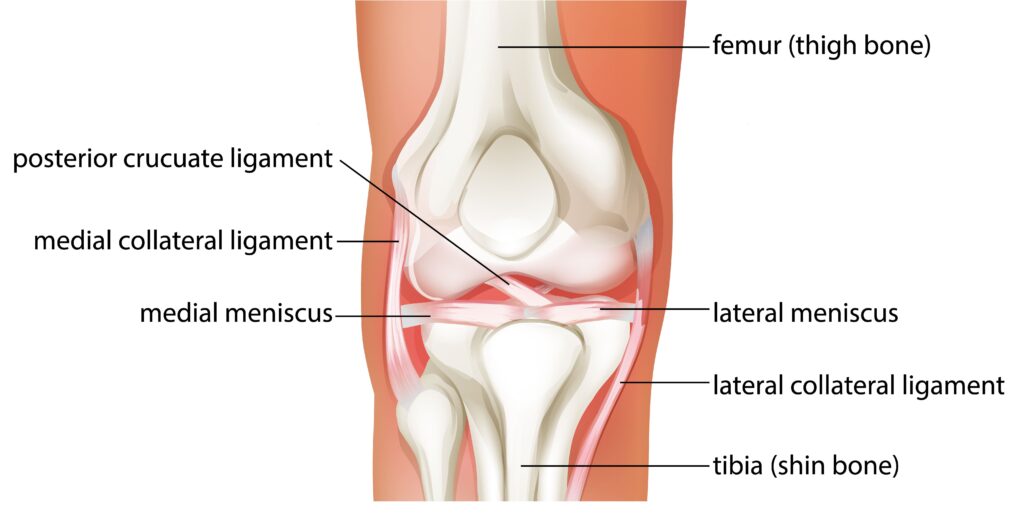
The meniscus is a C-shaped piece of cartilage that sits between the thigh bone (femur) and the shinbone (tibia). Each knee has two menisci, one on the inside (medial) and one on the outside (lateral) of the joint. The menisci provide cushioning, distribute weight, and help to stabilize the knee joint, allowing for smooth and painless movements.
The medial meniscus is larger and more prone to injury than the lateral meniscus. This is because the medial meniscus is firmly attached to the joint capsule and is less mobile than the lateral meniscus. Additionally, the medial meniscus is subjected to more stress during weight-bearing activities, making it more susceptible to tears and other injuries.
Functions of the Meniscus
The meniscus acts as a shock absorber, cushioning the joint from the impact caused by running, jumping, and other activities. Additionally, it helps to distribute weight evenly across the joint, reducing the strain placed on any one area. The meniscus also plays a crucial role in stabilizing the knee joint, helping to prevent dislocations and other injuries.
When the meniscus is damaged, it can no longer perform these functions effectively, leading to pain, swelling, and reduced mobility. In severe cases, surgery may be required to repair or remove the damaged meniscus.
Common Meniscus Injuries
Meniscus injuries can occur for a variety of reasons, including falls, sudden twists, and repetitive stress. The two most common types of meniscus injuries are tears and ruptures. Tears can be partial (where only part of the meniscus is damaged) or complete (where the entire meniscus is torn). Ruptures occur when the whole meniscus is completely detached from the knee joint.
Seek medical attention if you suspect you have a meniscus injury, as delaying treatment can lead to further damage and complications.
Types of Meniscus Surgery
The meniscus is a C-shaped piece of cartilage that helps cushion and stabilize the knee joint. When the meniscus is damaged, it can cause pain, swelling, and limited mobility. Meniscus surgery is a common treatment option for patients with meniscus injuries. There are several types of meniscus surgery, each with its own benefits and risks.
These procedures are performed arthroscopically with keyhole incisions in a minimally invasive fashion. Patients can go home on the same day or the day after.
Meniscectomy
In this procedure, the surgeon removes part of the damaged meniscus. This procedure is recommended for patients with tears or damage to the parts of the meniscus with poor blood supply and/or for meniscus tears that are not repairable.
During a meniscectomy, the surgeon will make a small incision in the knee and use specialized tools to remove the damaged tissue. Recovery time is generally quick, and patients can often return to light activity within a few weeks. However, because the meniscus is an important shock absorber for the knee joint, removing too much of it can lead to increased wear and tear on the joint and an increased risk of arthritis.
Meniscus Repair
Meniscus repair is the preferred option for patients with repairable tears with good blood supply. During this procedure, the surgeon will sew the torn edges of the meniscus back together with specialised meniscus repair devices.
Meniscus repair is a more complex procedure than a meniscectomy, and recovery time may be longer. Patients must be careful to avoid placing too much weight or pressure on the joint while it heals, which can take several weeks to months. Meniscus repair is the preferred option over menisectomy when possible.
Meniscus Transplant
In some cases, the meniscus may be damaged beyond repair, or a previous meniscectomy may have led to significant joint degeneration. In these instances, a meniscus transplant may be recommended. During the procedure, the surgeon will replace the damaged meniscus with a donor meniscus.
Meniscus transplant is a complex procedure that requires a compatible donor and careful post-operative care. Recovery time is longer than for other types of meniscus surgery, and patients will need to undergo ongoing physical therapy to ensure a successful outcome. However, for patients with significant meniscus damage, a meniscus transplant can help restore mobility and reduce pain.
Preparing for Meniscus Surgery
Diagnostic Tests
Before scheduling meniscus surgery, your doctor will likely order an MRI or other diagnostic test to determine the extent of the damage. This will help them determine which type of surgery is necessary and develop a plan for your recovery.
The MRI will allow your doctor to see the extent of the damage to your meniscus. They will be able to see the size and location of the tear, as well as any other damage that may have occurred. This information will be crucial in determining the appropriate surgical procedure and developing a plan for your recovery.
Preoperative Consultation
Your surgeon will go over the details of the surgery, including what to expect during the procedure, the risks and benefits of the surgery, and what your specific recovery timeline will look like. You should use this time to ask any questions you may have about the procedure or your recovery. Your surgeon will be able to provide you with detailed information and help alleviate any concerns you may have.
Pre-surgery Exercises
Depending on the severity of your injury, your doctor may recommend that you do specific exercises before surgery to help build strength in the area and prepare your body for the operation. This could include exercises to strengthen the surrounding muscles, such as the quadriceps, or stretches to increase flexibility.
These exercises are designed to help improve your range of motion and build strength in the muscles surrounding your knee. This can help improve your recovery time and reduce the risk of complications during and after surgery.
Preparing for Surgery
In the days leading up to your surgery, there are a few things you can do to prepare yourself:
- Make sure you have someone who can drive you to and from the hospital on the day of your surgery.
- Fill any prescriptions your doctor may have given you for pain medication or antibiotics.
- Arrange for someone to help you with daily tasks, such as cooking and cleaning, during your recovery period.
- Make sure you have loose-fitting clothing that will be comfortable to wear after your surgery.
The Meniscus Surgery Procedure
Anesthesia Options
Meniscus surgery can be performed under general anaesthesia or regional anaesthesia, depending on the extent of the procedure and your specific needs. Your surgeon will discuss your anaesthesia options with you during your preoperative consultation.
Surgical Techniques
The specific surgical technique used during your procedure will depend on the type of meniscus surgery you are undergoing. Generally, the surgery will involve making a small keyhole incision in the knee and using specialized tools to remove or repair the damaged meniscus.
Intraoperative Care
During the surgery, your care team will closely monitor your vitals and ensure that you are comfortable throughout the procedure. After the surgery is complete, you will be moved to a recovery area, where you will be monitored until you are ready to go home.
Recovery from Meniscus Surgery
In general, patients can expect to need several days to a week of rest before returning to light activity. Depending on your specific needs and the advice of your surgeon, you may need to undergo physical therapy to rebuild strength and flexibility in the joint.
Immediate Post-Op (0-48 hours):
During the first 48 hours after surgery, the focus is on managing pain and swelling. Patients can typically expect to ice and elevate their leg and wear a knee brace or immobilizer for support. Crutches are typically used for support during this time. Gentle range-of-motion exercises may be introduced to promote healing and prevent stiffness.
Early Recovery (Days 3-7):
In the first week, patients will gradually increase weight-bearing activities and continue managing pain and swelling. Gentle stretching exercises are introduced, and individuals may begin using a stationary bike or continuous passive motion (CPM) machine to help regain range of motion. Your specialist may also recommend you to keep an eye on the incision site for any signs of infection during this period.
Short-Term Recovery (Weeks 1-3):
During weeks 1-3, individuals can expect to return to normal daily activities gradually.A follow-up appointment with the surgeon usually occurs within this time frame. Based on the surgeon’s evaluation & recommendation, physical therapy sessions will begin, focusing on range-of-motion and strengthening exercises. Ice and compression may still be used for pain relief.
Mid-Term Recovery (Weeks 4-6):
As patients enter weeks 4-6, the intensity of the physical therapy will increase. Progressive strengthening exercises are introduced, and individuals may start low-impact aerobic activities, such as swimming or cycling. Depending on the individual’s progress, crutches may no longer be necessary. Regular follow-ups with the patient’s orthopaedic surgeon will continue during this phase.
Long-Term Recovery (Weeks 7-12):
From weeks 7 to 12, individuals will transition to more advanced exercises and gradually return to higher-impact activities like jogging and jumping. Patients may be recommended to focus on improving balance and coordination, and continue strengthening the surrounding muscles.
Full Recovery (Months 3-6):
Full recovery typically occurs between months 3 and 6, allowing individuals to resume most pre-injury activities and sports. Maintenance of strength and flexibility remains crucial, and individuals should continue monitoring their knee for any complications. The intensity and duration of physical activities can be gradually increased, with a final follow-up with the surgeon, if necessary.
Keep in mind that the recovery timeline may vary based on individual factors, the type of meniscus surgery, and the severity of the injury. Consult with your orthopaedic specialist for personalised recovery instructions and timelines.
Conclusion
The meniscus is an essential component of the knee joint that plays a crucial role in shock absorption, weight distribution, and joint stabilization. Injuries to the meniscus can be debilitating, and the severity of the injury dictates the appropriate treatment and recovery approach.
Meniscus surgery is a common treatment option for significant injuries and includes meniscectomy, meniscus repair, and meniscus transplant procedures. Preoperative preparation, personalized surgical techniques, and diligent postoperative care can all contribute to a successful outcome.
Recovery from meniscus surgery is a gradual process that can range from several weeks to six months, depending on the type of surgery and individual factors. Patients must follow their orthopaedic specialist’s guidance and remain committed to physical therapy and rehabilitation to ensure the best possible outcome.
In the long run, a successful meniscus surgery can alleviate pain, restore mobility, and allow patients to return to their pre-injury activities, improving their overall quality of life.